Changes To Medicaid “Eligibility & Enrollment” Aren’t Getting Much Attention, But We Shouldn’t Lose Sight Of Potentially Negative Impacts On Kids And Families
 By Dr. Heather Bomsta, Vice President of Policy & Programs, Michigan’s Children
By Dr. Heather Bomsta, Vice President of Policy & Programs, Michigan’s Children
May 13, 2025 – Medicaid cuts are still being debated, and we don’t know what form cuts will ultimately take, but there is one area of policy that we’re watching with special relevance to kids. “Eligibility and enrollment” sound dry and not very important – but it matters a lot to families. Eligibility and enrollment define who is eligible and how people access a program. Seemingly small changes in these policies can have real-world impact.
Currently, children (and caregivers) enrolled in Medicaid only recertify their eligibility once a year. The Energy & Commerce Committee is proposing that eligibility be checked twice a year. Sounds like a small change, but if a parent misses a letter (and what working parent doesn’t now and again?) or fails to fill out every form perfectly – their children could lose coverage. The majority of people who lose Medicaid are dropped because of paperwork or processing errors – not because they are truly ineligible for the program. Most of these people then reapply and are again covered by the program – though the process can take months. This going in and out of Medicaid is called “churn” and it’s bad for kid’s health.
Kids who experience churn (unstable health coverage) are impacted in many ways: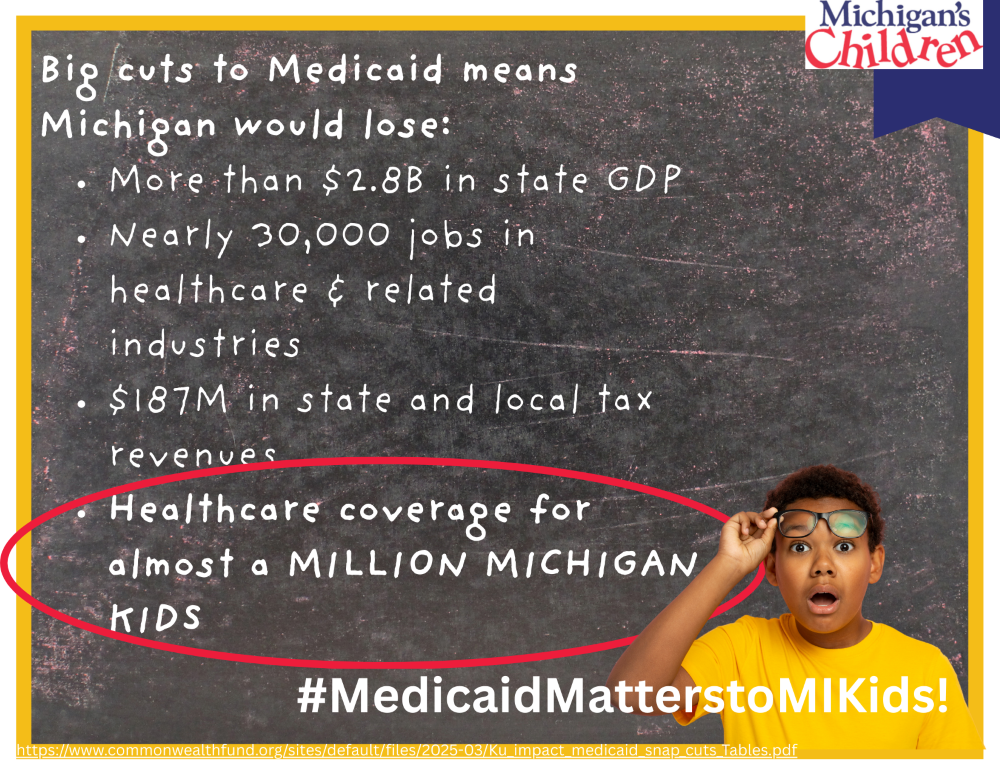
- Higher risk of growing up to be adults with chronic health problems – kids without health coverage have higher rates of disability and mortality as adults.1
- Less likely to get well-child/regular medical care – kids without health care coverage are more likely to miss regular check-ups. Missing regular healthcare interactions can mean these kids are sicker – and more expensive to treat – when they actually do get care. And parents covered by Medicaid are more likely to take their kids to healthcare providers than parents who don’t have health insurance, and this is especially true for low-income populations.2
- Less likely to diagnose and treat developmental and other delays/health issues early. Healthcare providers are trained to spot early childhood issues. Treating many developmental delays and other child health problems early can make a world of difference. Some developmental issues can be eliminated if treated early – setting a child up for success in school. Untreated delays and health issues become more serious and its harder to catch kids up – this can have lifelong impact.
- More likely to miss vaccinations. This leaves low-income kids at higher risk for serious childhood illnesses, like measles. Measles cases are on the rise in the US due to low vaccination rates and the US, for the first time in decades, has had several child deaths because of measles.
This is why some states adopted policies that provide “continuous coverage” for kids. Oregon, for example, has continuous coverage for kids from birth to age six and 24-months of continuous coverage for kids from six and up.3 The results from these states provided additional proof that providing every child with stable access to health care is good for kids and families and a good public investment.4 This eventually led to the US government instituting 12-month continuous coverage for kids as a federal policy.
The changes to eligibility being discussed now – going from 12-months of continuous coverage to only six months – would be a step backward for children in Michigan and nationwide.
Another change under discussion is removing the current policy that requires states to automatically move children from Medicaid to CHIP (or vice versa) when a caregiver’s income changes. It’s pretty common that income fluctuates in low-income families. Caregivers might find extra work some months of the year or be able to work more when kids are in school. Often the change isn’t a lot, but it can be enough that they no longer qualify for Medicaid. The Children’s Health Insurance Program (CHIP) was created to cover kids whose families make too much to qualify for Medicaid but still don’t make enough to pay for private health insurance.
Current US policy requires states to be instituting systems to automatically switch kids from one program to the other.5 This works beautifully for low-income families where parents are often juggling multiple jobs, child care, housing insecurity and a host of other challenges. Kids keep their coverage, and parents can take advantage of opportunities to earn a little more without worrying that a few hours of overtime might cause their kids to lose their health care access.
The House Energy & Commerce Committee has proposed amending this requirement for states – so they would not have to institute automatic switchovers until 2035. Delaying the requirement for states to implement these family-positive eligibility and enrollment provisions until 2035 would make life more difficult for lower-income families and result in more kids experiencing healthcare churn.
Families in states that don’t have this automatic changeover between Medicaid and CHIP – often have to apply for CHIP several times a year and then turn around – when income drops – and apply to Medicaid. And often this leads to coverage gaps for kids – as application processing could take weeks to months, and any paperwork errors could mean starting the process all over. These policies make things harder for families and result in poorer health outcomes for kids due to instability in health care coverage (churn). Why should kids and families in one of the most developed nations on earth have to wait 10 more years for something that can be done today (and is already done in some states)?
Current US policy also helped families by covering medical expenses retroactively – up to 90 days. This meant that if a kid broke an arm during a coverage gap – once they were approved for Medicaid or CHIP any expenses in the three months prior to their application would be covered. This helps families avoid medical debt – which can spiral low-income families deeper into poverty. The policy also helps health care providers (hospitals, doctors, etc.) who treat injured kids get paid and keep their doors open for all families. The current house draft limits the retroactive coverage to 30 days6 – again, making it harder for families and providers. Changing the retroactive coverage provision would hurt kids, families, and our healthcare system.
Eligibility and enrollment sound less important, but they matter a lot to kids and families – especially to the most vulnerable kids and families. Low-income caregivers are balancing so much – adding more paperwork, and less flexibility to Medicaid/CHIP will make these families more stressed and less healthy. Let’s not go backward – a country that values kids and families should keep Medicaid/CHIP eligibility and enrollment as streamlined as possible. The wealthy will still be wealthy – even without additional tax cuts – but kids can suffer lifelong consequences from not having reliable access to health care. Tell Congress to prioritize child and family health and wellness over tax cuts for the wealthy few.
Actions You Can Take:
- Call your US Representatives and leave a message telling them Medicaid enrollment & eligibility should be family-friendly and put kid’s health first! Call your US Senator, too! They will be voting on Medicaid as well – be sure they know that streamlining Medicaid enrollment & eligibility should be prioritized – not delayed. Family values mean children’s health should be prioritized above tax breaks for the wealthy.
- Find your US congressional members’ office numbers here: https://www.congress.gov/members/find-your-member
- Send an email to your congress members about Medicaid eligibility & enrollment here: https://actionnetwork.org/letters/tell-your-legislator-that-medicaid-processes-should-be-family-friendly-for-kids-sake?source=direct_link&
- Learn more and support Protect MI Care – a coalition of Michigan organizations working to protect Medicaid for Michigan kids, families, jobs, businesses, communities, hospitals and economy! https://protectmicare.org
_________________________
- Goodman-Bacon. (2021). The Long-Run Effects of Childhood Insurance Coverage: Medicaid implementation, adult health, and labor market outcomes. The American Economic Review, 111(8), 2550–2593. https://doi.org/10.1257/aer.20171671. pp. 15-16 ; Thompson, O. (2017). The Long-term Health Impacts of Medicaid and CHIP. Journal of Health Economics, 51, 26-40. https://pubmed.ncbi.nlm.nih.gov/28040620/
- Center on Budget and Policy Priorities. (2020, October). The Far-reaching Benefits of the Affordable Care Act’s Medicaid Expansion. https://www.cbpp.org/research/health/chart-book-the-far-reaching-benefits-of-the-affordable-care-actsmedicaid-expansion
https://www.kff.org/policy-watch/section-1115-waiver-watch-continuous-eligibility-waivers/ - https://www.kff.org/policy-watch/section-1115-waiver-watch-continuous-eligibility-waivers/
- Brantley, E., & Ku, L. (2022). Continuous Eligibility for Medicaid Associated with Improved Child Health Outcomes. Medical
Care Research and Review, 79(3), 404-413. - Currently the House is discussing amending this – so that states would not have to comply with this provision until 2035.
- https://www.kff.org/tracking-the-medicaid-provisions-in-the-2025-budget-bill/?utm_campaign=KFF-Medicaid
